For the millions living with diabetes or at risk of developing the condition, regular blood glucose monitoring is the cornerstone of effective health management. For decades, finger-prick glucose meters have been the go-to tool for this task—but they come with a host of drawbacks that often hinder consistent, long-term monitoring. In contrast, the emergence of non-invasive glucose meters has revolutionized this daily routine, combining cutting-edge technology with user-centric design to deliver a superior experience that prioritizes comfort, adherence, and accuracy. This article explores the key differences between these two devices, with a focus on the transformative advantages of non-invasive glucose monitoring.
Traditional finger-prick glucose meters operate on a simple yet invasive principle: a sharp lancet pierces the fingertip to draw a small drop of capillary blood, which is then placed on a disposable test strip for analysis. While these devices are relatively affordable and widely available, their limitations are impossible to ignore. First and foremost is the pain and discomfort associated with repeated lancing. For many users—especially children, adolescents, and the elderly—this physical distress translates into anxiety and reluctance to test regularly. Studies have shown that up to 30% of diabetes patients skip or delay glucose checks due to fear of finger pricks, leading to inconsistent data that undermines the ability to adjust medication, diet, or exercise plans effectively.
Beyond pain, finger-prick meters pose other practical challenges. The risk of skin irritation, infection, and scarring increases with frequent use, particularly for those with sensitive skin or poor circulation. Disposable test strips add to the long-term cost burden, and their need for careful storage (away from heat and moisture) makes them inconvenient for on-the-go use. Additionally, the process is time-consuming: lancing the finger, waiting for a sufficient blood sample, and disposing of used lancets and strips creates friction in busy daily schedules, further discouraging regular monitoring.
Non-invasive glucose meters, by contrast, eliminate all these pain points by leveraging advanced technologies that require no skin puncture whatsoever. The most common approaches include near-infrared spectroscopy (NIRS), radiofrequency impedance, and transdermal fluid extraction—all designed to detect glucose levels in interstitial fluid beneath the skin’s surface without breaking the epidermis. NIRS-based devices, for example, emit low-intensity infrared light that penetrates the outer skin layer; the light interacts with glucose molecules, and the device calculates blood glucose levels by measuring resulting wavelength shifts with medical-grade precision. Other models use gentle electrical currents or vacuum pressure to draw tiny amounts of interstitial fluid through microchannels too small to stimulate nerve endings, ensuring a completely pain-free experience.
The advantages of non-invasive meters extend far beyond comfort, making them a game-changer for diabetes management. The most significant benefit is dramatically improved monitoring adherence. Research indicates that users of non-invasive devices test their blood glucose 30–40% more frequently than those relying on finger-prick meters. This consistency is critical: it allows for real-time tracking of glucose fluctuations, early detection of hyperglycemia or hypoglycemia, and timely adjustments to treatment plans—all of which reduce the risk of life-threatening complications such as nerve damage, kidney failure, and cardiovascular disease.
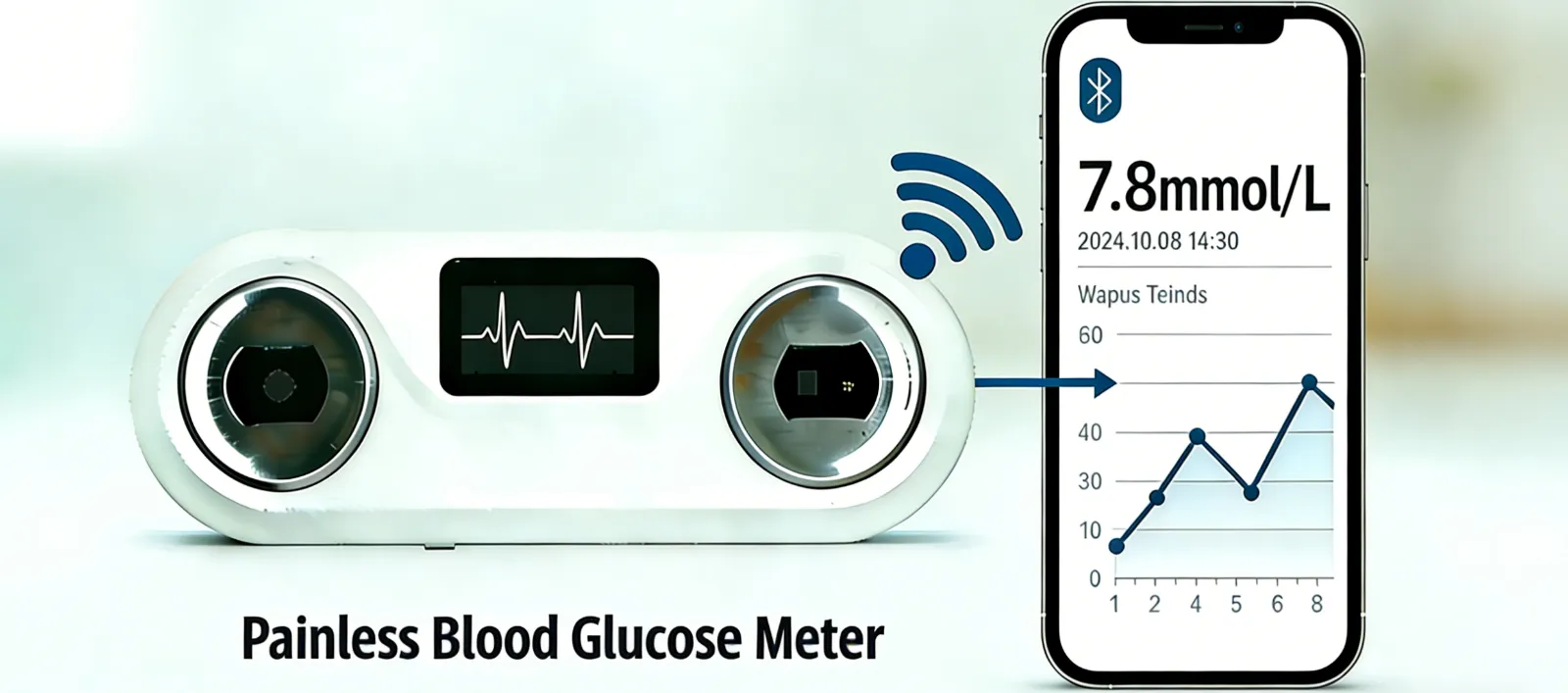
Convenience is another standout feature of non-invasive glucose meters. Most models are compact, portable, and rechargeable, eliminating the need for test strips or lancets entirely. Many sync seamlessly with smartphones, enabling users to log data, set reminders, and share insights with healthcare providers remotely. Some advanced devices even offer continuous glucose monitoring (CGM) capabilities, providing 24/7 real-time data without any manual intervention—a feature that is transformative for athletes, busy professionals, and parents monitoring children with diabetes.
Non-invasive meters also address the cost and sustainability concerns of traditional devices. While their upfront price tag may be higher, the absence of disposable test strips and lancets significantly reduces long-term expenses. This makes them a more economical choice over time, especially for users who require multiple daily tests. Moreover, the elimination of single-use plastics aligns with global sustainability goals, reducing medical waste associated with diabetes care.
From a user experience perspective, non-invasive meters are far more inclusive. They are ideal for children and adolescents, who often struggle with the anxiety of finger pricks, as well as elderly users with fragile skin or limited dexterity. For athletes and fitness enthusiasts, the ability to monitor glucose levels during workouts without interruptions or discomfort helps optimize performance and nutrition. The non-invasive design also reduces the risk of infection—a crucial benefit for those with compromised immune systems or poor wound-healing abilities.
It is worth noting that early non-invasive models faced criticism for slightly lower accuracy compared to finger-prick devices, especially in extreme glucose ranges. However, technological advancements have narrowed this gap significantly. Modern non-invasive meters use advanced algorithms and machine learning to calibrate readings, meeting the strict accuracy standards set by regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the International Organization for Standardization (ISO). For most users, the difference in accuracy is negligible, and the benefits of consistent monitoring far outweigh this minor trade-off.
In conclusion, while finger-prick glucose meters have served as a vital tool for diabetes management for decades, they are increasingly being overshadowed by the superior performance of non-invasive alternatives. Non-invasive glucose meters eliminate pain and discomfort, boost monitoring adherence, reduce long-term costs, and offer unparalleled convenience—all while maintaining the accuracy needed for effective health management. As technology continues to evolve, these devices will play an even more central role in empowering individuals with diabetes to take control of their health, leading to better outcomes, improved quality of life, and a future where glucose monitoring is no longer a source of stress, but a seamless part of daily self-care.